
A Plan for Treatment of White Phosphorous Casualties
- Posted by Mike Shertz MD/18D
- Categories Tactical CBRN
🕖 Reading Time, 10 minutes
With the Russian invasion of Ukraine, there have been discussions about the management of casualties injured by white phosphorous munitions.
A social media post by @nardoctor sharing the DOD clinical practice guidelines was one of the first to address this topic. It made us interested in the medical literature supporting the management of these casualties.
White phosphorous is a solid, chalk-like, waxy material used in many military munitions to include hand grenades, mortar rounds, artillery, and bombs. It has been involved in many other recent conflicts. Over the past 15 years alone, it has been used in Iraq, Syria, Afghanistan, Yemen, Azerbaijan, and Gaza.
Typically classified as an incendiary agent, white phosphorus is also used as an obscurant for its ability to generate a thick white cloud of smoke that may interfere with IR imaging and weapon tracking devices.1
When white phosphorous encounters air it ignites, burning as a bright yellow flame. Many have described it as smelling like garlic, which could be confused with the chemical warfare agent sulfur mustard, which is also described as smelling like garlic, onions, or mustard.
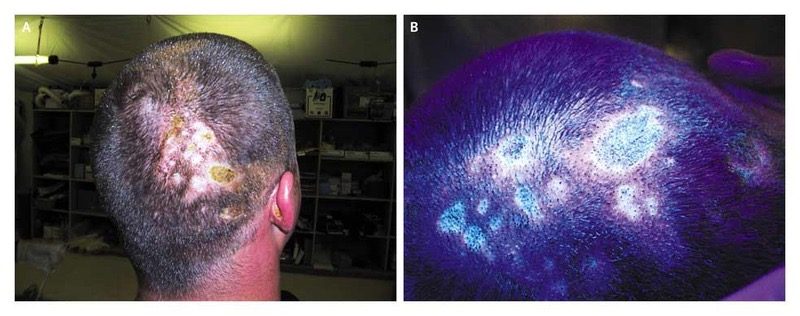
White phosphorous continues to burn if exposed to oxygen or until it has completely consumed itself. The burning white phosphorous particles can become embedded in human skin where they continue to burn.

A 12 to 15% white phosphorous total body surface area burn (TBSA) can be fatal in experimental models.3 In humans, fatalities from white phosphorous burns have occurred with less than 10% TBSA involvement.4
All contaminated clothing needs to be removed as soon as possible. To extinguish the ignited white phosphorous, it needs to be deprived of oxygen. This is best done with immersion in cool water or covering the burning area with water / saline moistened dressings.
Because white phosphorous particles become liquid at 44 degrees Celsius, warm or hot water will exacerbate the wounds by liquifying it, causing it to run over a larger surface area, thereby increasing the amount of burned tissue. Similarly, aggressive water irrigation can splash the white phosphorous particles to unburned tissue and rescuers only to ignite once the particles dry out.5 Some have stated that “extinguishing burning phosphorous with a stream of water is dangerous and ineffective.”6 However, tap water irrigation, best performed in the field, is the only treatment consistently documented to decrease death from white phosphorous burns, the severity of the burn, and length of hospitalization.7 These factors would seem to indicate there is a role for irrigation, but perhaps after moistened gauze was used to extinguish the burning particles. Caution would still be needed to decrease a splash risk to the casualty and rescuers. There is a documented case when during wound debridement, a white phosphorous particle dislodged and burned a nurse’s neck.8

Debridement of sloughed skin and removal of obvious phosphorous particles from the skin are crucial techniques to limit wound severity and systemic absorption of phosphorous and may be best performed prehospital.9 Unfortunately, excision of the burned area one hour after exposure has not been shown to decrease mortality, suggesting it might need to be done even sooner after injury to be beneficial.10
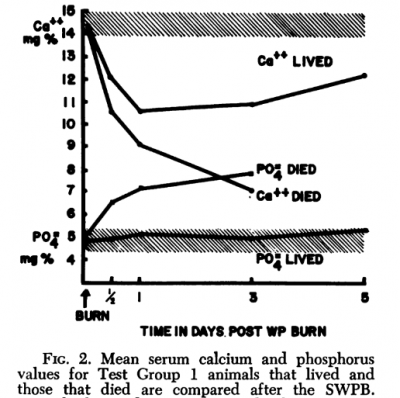
There is speculation the increased mortality, compared to a similarly sized thermal burn, is secondary to absorption of phosphorous, which can result in elevated phosphorus levels, decreased calcium, and subsequent cardiac rhythm abnormalities. In the study of New Zeland white rabbits, they checked these levels and EKGs every hour for the first twelve hours.4
Additionally, the phosphorous can cause liver necrosis and direct renal damage ultimately resulting in kidney failure. In a Chinese study of 81 casualties from a yellow phosphorous explosion, where the average TBSA burn was 9%, disproportionally full-thickness, 33% had liver dysfunction, 18.5% kidney injury, and 52% electrolyte disturbances.11
Standardized fatal white phosphorous burns on New Zealand while rabbits showed significant hypocalcemia and hyperphosphatemia as early as one-hour post-burn. 4
Like hydrofluoric acid burns, which can also result in similar electrolyte disturbances and dysthymias, white phosphorous burned casualties should be monitored in a hospital setting, even for small burns.
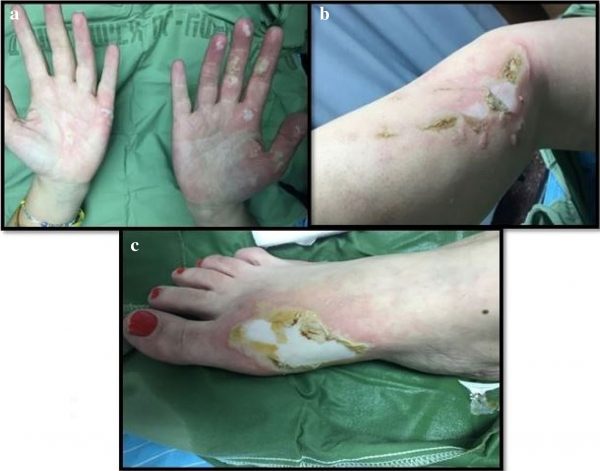
In a study of 87 soldiers injured by white phosphorous from the Nagorno-Karabakh war in 2020, between Azerbaijan and the Republic of Artsakh, the average TBSA burned was 14%. Head and neck burns occurred in nearly 80% of casualties. Upper extremities and hand burns in 90%. More traditional fragment wounds were found in 38%.12
A Polish military study evaluated the ability of five “first aid dressings” to extinguish flame, eliminate white phosphorous from a surface, and prevent re-ignition.13 They conducted 1,100 experiments with white phosphorous placed on a piece of military uniform on top of raw bacon. They then tested the various “first aid dressings.” Moistened gauze was very efficient at extinguishing flame. It also removed and absorbed a significant amount of the white phosphorous, preventing deeper burns, and eliminating re-ignition. It outperformed all the manufactured dressings tested. Many of the other dressings were poor at preventing re-ignition as they didn’t absorb or remove the particles. Some actually worsened the burn injury.
Possible Treatment Plan: An ideal scenario
This is an ideal treatment plan, recognizing in conflict zones, ideal doesn’t always happen.
Step 1: Remove all contaminated clothing
Step 2: Submerge or immerse white phosphorous burn in cool water (if possible)
Step 3: Remove all embedded white phosphorous particles by pressing moistened gauze for 3-5 minutes; (obvious particles will need to be removed with forceps)
Step 4: Debride all sloughed skin
Step 5: Dress all burns with cool, moistened gauze, keep wet during transport
Step 6: Water Jel WJ110 could be placed on the wound for transport, if keeping the gauze wet is not possible
Step 7: Monitor calcium, phosphorous levels, EKG changes, hourly for the first 12-hours, and watch for organ failure

NOTES:
1 Berndtson AE, Fagin A, Sen S, Greenhalgh DG, Palmieri TL. White phosphorus burns and arsenic inhalation: a toxic combination. J Burn Care Res. 2014 Mar-Apr;35(2):e128-31.
2 Barqouni L, Abu Shaaban N, Elessi K. Interventions for treating phosphorus burns. Cochrane Database Syst Rev. 2014 Jun 4;2014(6):CD008805.
3 Ben-Hur N, Giladi A, Neuman Z, Shugerman B, Applebaum J. Phosphorus burns–a pathophysiological study. Br J Plast Surg. 1972 Jul;25(3):238-44.
4 Bowen TE, Whelan TJ Jr, Nelson TG. Sudden death after phosphorus burns: experimental observations of hypocalcemia, hyperphosphatemia and electrocardiographic abnormalities following production of a standard white phosphorus burn. Ann Surg. 1971 Nov;174(5):779-84.
5Aviv U, Kornhaber R, Harats M, Haik J. The burning issue of white phosphorus: a case report and review of the literature. Disaster Mil Med. 2017 Aug 30;3:6.
6Witkowski W, Surowiecka-Pastewka A, Biesaga M, Gierczak T. Experimental Comparison of Efficiency of First Aid Dressings in Burning White Phosphorus on Bacon Model. Med Sci Monit. 2015 Aug 12;21:2361-6.
7Davis KG. Acute management of white phosphorus burn. Mil Med. 2002 Jan;167(1):83-4.
8 Al Barqouni LN, Skaik SI, Shaban NR, Barqouni N. White phosphorus burn. Lancet. 2010 Jul 3;376(9734):68.
9Davis KG. Acute management of white phosphorus burn. Mil Med. 2002 Jan;167(1):83-4.
10Chou TD, Lee TW, Chen SL, Tung YM, Dai NT, Chen SG, Lee CH, Chen TM, Wang HJ. The management of white phosphorus burns. Burns. 2001 Aug;27(5):492-7.
11Xie WG, Huang WW, Yao SG, Wang DY, Wang MX, Zhu ZQ, Liu JF, Zhang W. [Rescue and treatment for the mass burn casualties of yellow phosphorus explosion]. Zhonghua Shao Shang Za Zhi. 2008 Feb;24(1):36-8.
12Brutyan S, Babayan K, Barseghyan N, Petrosyan V, Knipper P, Bégué T, Khachatryan L, Khonsari RH. Evidence for chemical burns by white phosphorus in Armenian soldiers during the 2020 Nagorno-Karabakh war. Injury. 2021 Apr;52(4):1100-1101.
13Witkowski W, Surowiecka-Pastewka A, Biesaga M, Gierczak T. Experimental Comparison of Efficiency of First Aid Dressings in Burning White Phosphorus on Bacon Model. Med Sci Monit. 2015 Aug 12;21:2361-6.
Dr. Mike Shertz is the Owner and Lead Instructor at Crisis Medicine. Dr. Shertz is a dual-boarded Emergency Medicine and EMS physician, having spent over 30 years gaining the experience and insight to create and provide his comprehensive, science-informed, training to better prepare everyday citizens, law enforcement, EMS, and the military to manage casualties and wounded in high-risk environments. Drawing on his prior experience as an Army Special Forces medic (18D), two decades as an armed, embedded tactical medic on a regional SWAT team, and as a Fire Service and EMS medical director.
Using a combination of current and historical events, Dr. Shertz’s lectures include relevant, illustrative photos, as well as hands-on demonstrations to demystify the how, why, when to use each emergency medical procedure you need to become a Force Multiplier for Good.



