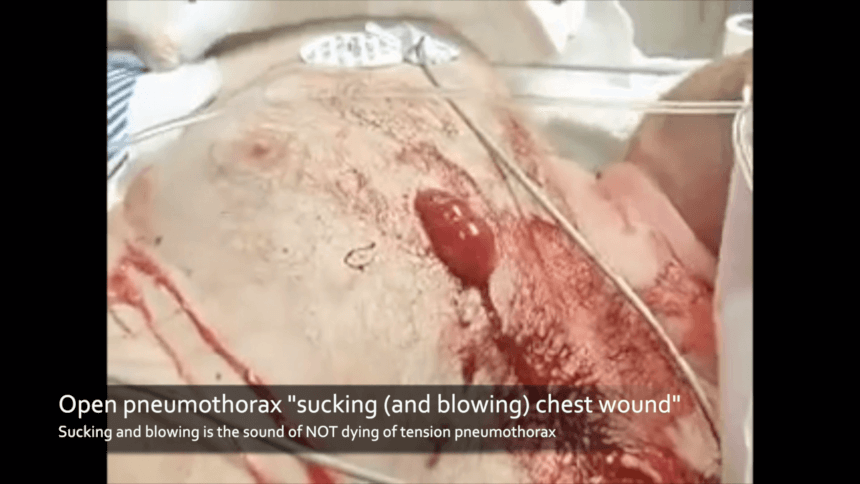
A sucking (and blowing) chest wound is the sound of not dying
- Posted by Mike Shertz MD/18D
- Categories (R) Respiration
Video used with permission by Andrew Dennis, DO FACS, FACOS, Cook County Trauma Burn Unit, Chicago Il
🕖 Reading Time, 6 minutes
Sucking chest wounds are dramatic, but rarely life-threatening.
The sound of sucking & blowing is the sound of not dying of tension pneumothorax.
There is no good evidence an open pneumothorax needs to be sealed and you can cause tension.
Although the open pneumothorax or “sucking chest wound” is dramatic in appearance, it is rarely fatal. TCCC Guideline change 13-02 noted, “there were no fatalities during OEF and OIF attributed to isolated open pneumothorax.”1
Described succinctly in a 1964 publication: “If a wound in a chest wall communicates with the pleural cavity, there is usually an audible passage of air during both phases of respiration.”2
The principle here is although air enters the chest wall defect (eg, a gunshot wound) during inspiration, it also blows out on expiration. These sounds of the wound both sucking and blowing is the sound of not dying of tension pneumothorax.
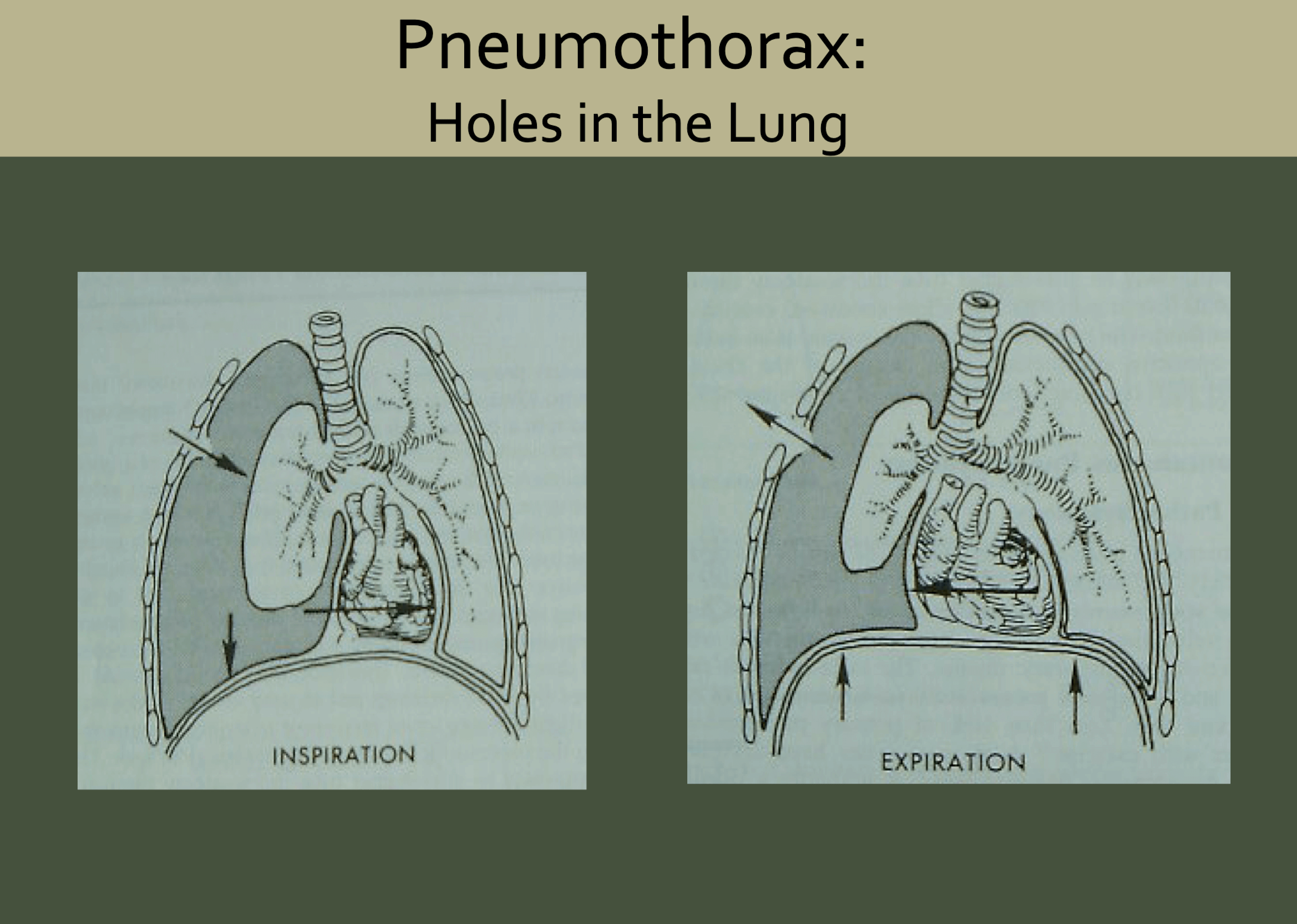
Tension Pneumothorax
A tension pneumothorax, on the other hand, can be fatal. Here, air enters the chest outside the lung but does not escape. As more air accumulates inside the chest, but outside of the actual lung, it creates increased pressure within the thorax which interferes with both heart and uninjured lung function.
“Progressive accumulation of air in the pleural space and the decrease in oxygen saturation does not appear to influence the mean arterial pressure and heart rate until involvement by pneumothorax of approximately 47% of total lung capacity.”3 With an average adult total lung capacity of 6 liters, clinically significant tension pneumothorax won’t occur until nearly 3 liters of air accumulates in the injured hemithorax.
In 1945, Synder et all noted sealing an open pneumothorax had the potential to develop tension pneumothorax from an underlying lung injury and air leak.4 Additionally, the International Liaison Committee on Resuscitation First Aid Task Force 2015 guidelines also did not support the application of an occlusive dressing to open chest wounds.5
The problem is not the hole in the chest wall letting air in, because it usually also lets air out. Once the chest wall defect is occlusively sealed, air can’t escape. If there is an underlying lung injury and air leak causing air to re-accumulate, it can’t escape from the hole you just sealed. This can cause tension pneumothorax and death.
Three-sided Occlusive Dressing Myth
Before the advent of commercial chest seals, an improvised, three-sided occlusive dressing, made with petrolatum gauze was recommended. However, this dressing has no clear human or animal literature to show it ever worked. One study from 1993 compared a “low profile, one-way valve dressing” with a “traditional occlusive petrolatum gauze dressing” in 8 dogs. Each dog had a 6 mm plastic sleeve placed into each side of the chest to simulate bilateral open pneumothoraces. The “traditional” petrolatum gauze dressing failed in all 8 spontaneously breathing dogs.6
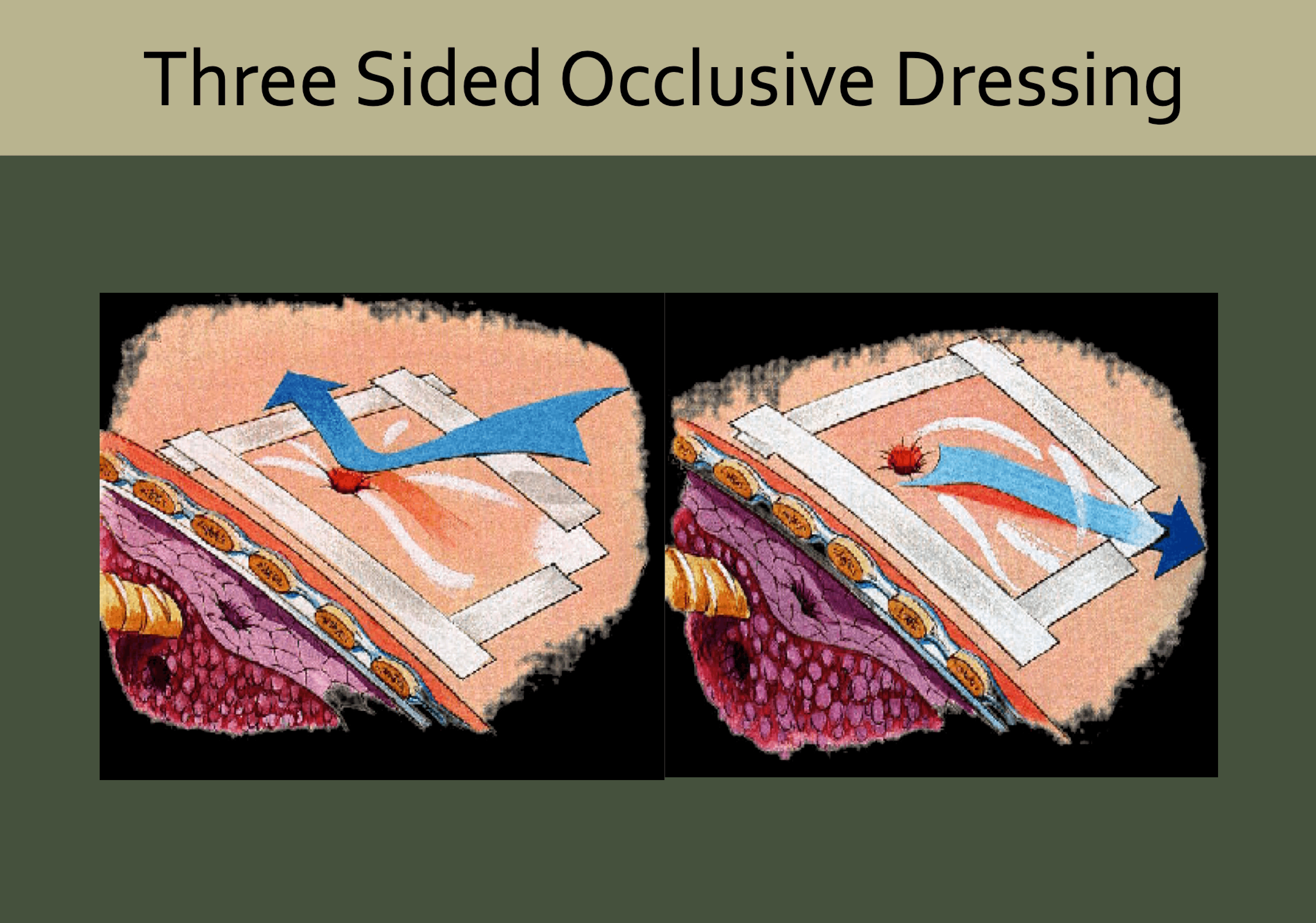 Ruiz et al intended the petrolatum dressings to be completely occlusive (not the three-sided version which could theoretically let air out). However, they noted despite taping the dressing in place on all four sides, they were still not “airtight”.
Ruiz et al intended the petrolatum dressings to be completely occlusive (not the three-sided version which could theoretically let air out). However, they noted despite taping the dressing in place on all four sides, they were still not “airtight”.
In 2008 the TCCC committee removed the recommendation for placing improvised three-sided chest seals on casualties. After a literature review, they indicated there was no evidence the dressing prevented the conversion of an open pneumothorax to a tension pneumothorax. In 2013 after a subsequent review, they again could find no evidence the improvised dressing was “effective either in reversing the respiratory difficulty caused by an open pneumothorax or in preventing the conversion of an open pneumothorax into a tension pneumothorax.”7
Although there is experimental animal literature that vented (compared to non-vented) commercial chest seals do work to prevent an open pneumothorax with ongoing air leak from becoming tension pneumothorax,8,9,10 there still is no clear evidence that an isolated open pneumothorax needs to be sealed.
Seal it if the hole is 2/3 the size of the trachea?
In the prehospital environment, the oft-cited belief is ‘if the hole in the chest wall is 2/3 rds the size of the trachea it should be sealed.’ The stated theory behind this adage is the hole will be a more accessible conduit for air to enter into the thorax than through the trachea and into the lungs and thus must be sealed. For air to oxygenate your blood, it must be inside the lungs, not just inside the chest wall. Unfortunately, I cannot find the first time this statement was made in print, nor any evidence it is accurate or clinically relevant to the casualty.
Even if you buy into this simple approach, how do you operationalize it? The average human trachea is between 10 to 27 mm based on a study of 808 adults.11 That would mean you seal a chest wound if it is 6 mm in diameter in some cases and other times not until it is 18 mm?
Some claim the hole must be sealed because it “improves the mechanics of breathing.” Similarly, I can find no published literature showing any evidence that in an otherwise healthy individual, any sized unilateral chest wall defect needs immediately to be sealed.
The worst-case scenario with an open pneumothorax is a 100% collapse of that lung. Emergency Physicians routinely take care of patients with spontaneous pneumothoraces and 100% complete collapse of one lung with no significant vital sign abnormalities or significant resting shortness of breath.
If you choose to seal chest wounds, use a vented chest seal. If you want to go with the evidence and cut down on medical gear you carry, there just isn’t any compelling evidence penetrating chest injuries involving only one side of your casualty need to be sealed.
Interested to learn more? Try our online courses, or get started with a sample of the material in the preview course
TRAIN NOWOnline Tactical Casualty Care Classes
1Eastridge B, et al. Death on the battlefield (2001-2011): implications for the future of combat casualty care. J Trauma Acute Care Surg. 2012;73:S431– S437.
2Edgescombe E., et al. Principles of the early management of the patient with injuries to the chest. J Natl Med Assoc.1964;56:193-197
3Barton ED., et al. Tension Pneumothorax. Curr Opin Pulm Med. 1999 Jul;5(4):269-274
4Synder H., et al. The management of intrathoracic and thoracoabdominal wounds in the combat zone. Ann Surg 1945;122:333-357.
5Singletary EM., et al. 2015 International Consensus on First Aid Science With Treatment Recommendations. Circulation. 2015;132: S269-S311
6Ruiz E., et al. A one-way valve chest wound dressing: Evaluation in a canine model of open chest wounds
7Butler F.,et al. Management of open pneumothorax in Tactical Combat Casualty Care: TCCC Guidelines Change 13-02
8Kheirabadi BS.,et al.Vented versus unvented chest seals for treatment of pneumothorax and prevention of tension pneumothorax in a swine model. J Trauma 2013 Jul;75(1):150-6.
9Kotora JG.,et al. Vented chest seals for prevention of tension pneumothorax in a communicating pneumothorax. J Emerg Med 2013 Nov;45(5):686-94.
10Kheirabdai BS. et al. Do vented chest seals differ in efficacy? An experimental evaluation using a swine hemopneumothorax model. J Trauma and Acute Care Surg; 2017 Jul;83(1):182-189.
11Breatnach E.,et al. Dimensions of the normal human trachea. AJR Am J Roentgenmol. 1984 May;142(5):903-6.
Dr. Mike Shertz is the Owner and Lead Instructor at Crisis Medicine. Dr. Shertz is a dual-boarded Emergency Medicine and EMS physician, having spent over 30 years gaining the experience and insight to create and provide his comprehensive, science-informed, training to better prepare everyday citizens, law enforcement, EMS, and the military to manage casualties and wounded in high-risk environments. Drawing on his prior experience as an Army Special Forces medic (18D), two decades as an armed, embedded tactical medic on a regional SWAT team, and as a Fire Service and EMS medical director.
Using a combination of current and historical events, Dr. Shertz’s lectures include relevant, illustrative photos, as well as hands-on demonstrations to demystify the how, why, when to use each emergency medical procedure you need to become a Force Multiplier for Good.



