Does that Burn Casualty Need Intubation?
- Posted by Mike Shertz MD/18D
- Categories (A) Airway, More
Airway control remains the top priority for field treatment of burn casualties.1
🕖 Reading Time, 4 minutes

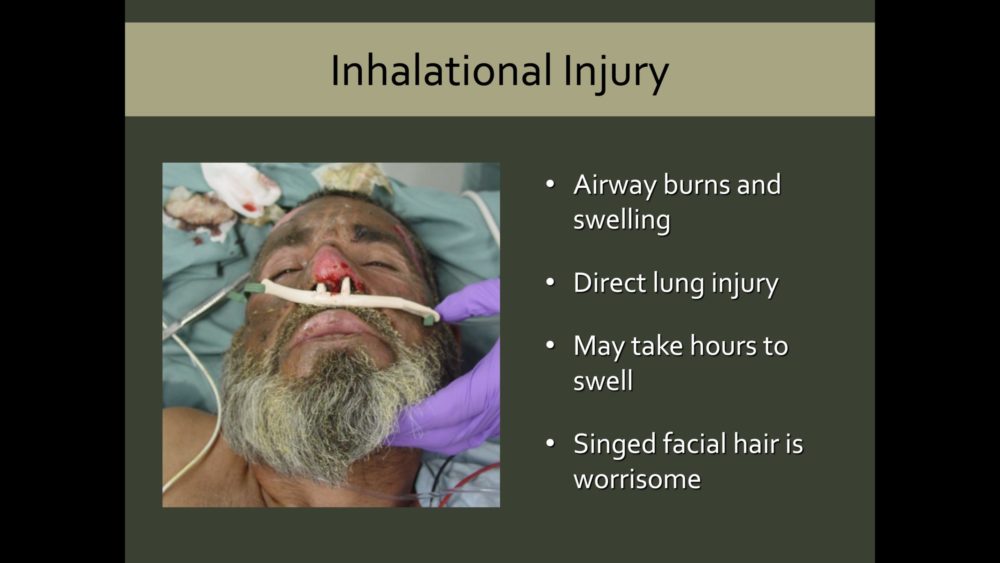
Hypovolemic and distributive shock can occur in burned patients but they are usually a late consequence. An inhalational burn injury can double a casualty’s burn mortality.2
Upper airway thermal injury can result in substantial tissue edema, with resulting airway occlusion and hypoxia. Between 20 to 33% of patients admitted with smoke inhalational injury may present with acute upper airway obstruction.3
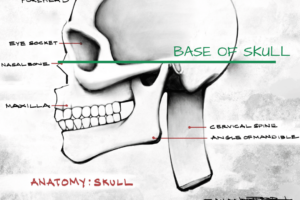
Suggestions of upper airway thermal injury include significant neck/facial burns, burns in the mouth, oropharyngeal soft-tissue edema, stridor, and abnormal voice. Soot in the mouth and singed nasal hairs may indicate potential airway involvement. Any burn in an enclosed space is concerning as well.
With progressive local inflammation, cell death, and increased capillary permeability, significant airway edema can occur after IV fluid resuscitation. This is often not predictable at the beginning of the resuscitation. Burns greater than 40% BSA will require substantial IV fluid administration with likely resultant edema, which can involve the airway. Some use this BSA cutoff as a marker for mandatory intubation.
A French study looked at the rate of difficult airways in patients with at least partial thickness or greater face/neck burns who were intubated prehospital (by EMS physicians) or at the burn center. Difficult airways were noted in 11.2% of their studied patients overall. They found intubation prehospital had a 3.5% difficult airway rate, compared to 16.9% of those intubated at the burn center. The patients had similar burn severity. The only difference was how soon after their burn they were intubated. The likelihood of a patient having a difficult airway tripled after two hours post-burn.4
One-quarter of the intubated patients in the French study were extubated in less than 24 hours suggesting they may not have required intubation.4 This study used data from 2007 to 2011. Since that time, there has been a sense in the burn community that the presence of facial burns alone is not a strong predictor of inhalational burn injury.5

It is challenging to integrate all of this information clinically. If we wait too long to intubate these patients, ie over two hours, the likelihood of a difficult airway triples. However, there is clear morbidity and potential mortality in intubating patients that ultimately don’t need it. That’s what continues to make this a challenging on the ground decision for pre-hospital providers.
As always, the need for airway control are imminent threat of airway obstruction, respiratory failure not responsive to other less invasive treatments, and altered mental status with a lack of airway protection.
References
1 Lin CH, Lin CH, et all, Challenges of Burn Mass Casualty Incidents in the Prehospital Setting: Lessons Learned from the Formosa Fun Coast Color Party, Prehosp Emer Care 2018;23:44-48
2 Sheppard NN, Hemington-Gorse S, Prognostic scoring system in burns: a review. Burns 2011;37:1288-95
3 Emergency Department Management of Smoke Inhalation Injury in Adults, Emergency Medicine practice, March 2018.
4 Esnault P, Prunet B, Tracheal intubation difficulties in the setting of face and neck burns: myth or reality? Am J Emerg Med 2014;32:1174-1178.
5 Kaneko T, Tanaka H, Predictors of Inhalational Burn Injury using Fire Site Information. Ann of Burn and Fire Disaster 2017; 30(4):275-277
Dr. Mike Shertz is the Owner and Lead Instructor at Crisis Medicine. Dr. Shertz is a dual-boarded Emergency Medicine and EMS physician, having spent over 30 years gaining the experience and insight to create and provide his comprehensive, science-informed, training to better prepare everyday citizens, law enforcement, EMS, and the military to manage casualties and wounded in high-risk environments. Drawing on his prior experience as an Army Special Forces medic (18D), two decades as an armed, embedded tactical medic on a regional SWAT team, and as a Fire Service and EMS medical director.
Using a combination of current and historical events, Dr. Shertz’s lectures include relevant, illustrative photos, as well as hands-on demonstrations to demystify the how, why, when to use each emergency medical procedure you need to become a Force Multiplier for Good.