Head to head: Doppler vs. Pulse oximeter as a training tool for tourniquet efficacy. Doppler wins.
- Posted by Mike Shertz MD/18D
- Categories (M) Massive Hemorrhage
🕖 Reading Time, 5 minutes
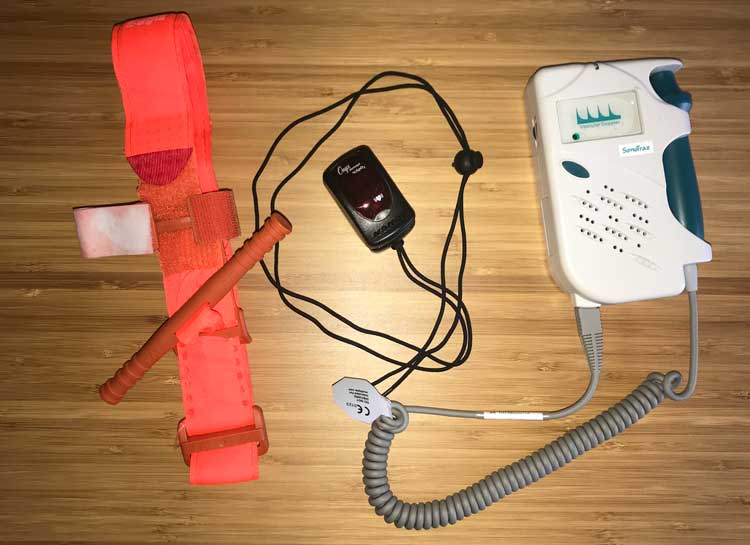
BLUF:* Is there a role for using a fingertip pulse oximeter as a training tool for tourniquet placement? We believe the answer is no. Considering the relative expense of a quality, FDA approved model pulse ox, a handheld doppler ultrasound is better, cheaper, provides audible pulsation feedback, and is the acknowledged standard.
Proper limb tourniquet application implies no arterial blood flow past the point of tourniquet application. In training, the loss of a palpable downstream pulse is often used as a marker of successful tourniquet tightness. However, an arterial pulse’s ability to be felt with fingers is lost long before the complete cessation of arterial flow through the artery.
As an example, although the exact numbers are argued, a radial pulse is no longer palpable when the arterial blood pressure through the artery drops below 80 mmHg.1 Although this is only 2/3 of normal blood pressure, it is far from no flow and in an injured artery would still represent substantial ongoing hemorrhage.
To improve accuracy and better understand how tightly tourniquets need to be placed to occlude arterial flow, some advocate using a fingertip pulse oximeter as a monitor of distal blood flow. However, pulse oximeters are designed to display accurate arterial oxygen saturations, not the presence of weak arterial flow.1
In a study by Wall, et al.2, three pulse oximeters were compared to doppler ultrasound for their ability to detect loss of arterial flow after volunteer tourniquet application to both arms and legs. None of the tested pulse oximeters were of the “fingertip” type. All were somewhat large monitors with the finger saturation probe attached to the monitor by wire cable. These tabletop models are more accurate versions than the pocket/aid bag friendly, Nonin-type, pulse oximeters.
As the tourniquet was tightened, in all of the pulse oximeter devices tested, the signal was lost before the doppler registered no detachable flow. When all three pulse oximeters were placed on the same limb, they corresponded with one another only 80% of the time as to whether a pulse was present.
The accuracy of the pulse oximeter readings were highly variable between monitors and in application to finger versus toes. In general, the devices were much less accurate on toes.
Interestingly, the sensitivity of the pulse oximeters varied between 75 to 92% compared to doppler. Their specificity was only 44 to 83%. A low specificity test means there are a lot of false-positive results. In this case, the oximeter read “no flow,” when actually, arterial flow persisted.
Dr. Wall’s study conclusion? Doppler is the de facto gold standard for noninvasive monitoring of tourniquet effectiveness.
Is there a role for using a fingertip pulse oximeter as a training tool for tourniquet placement? We believe the answer is no. Even a quality fingertip model shows decreased accuracy overall, and particularly on toes (high thigh tourniquet application having the highest failure rate in real-world applications). Considering the relative expense of a quality, FDA approved model pulse ox, a handheld doppler ultrasound is better, cheaper, provides audible pulsation feedback, and is the acknowledged standard.
Interested to learn more? Try our online courses, or get started with a sample of the material in the preview course
Preview CourseNot sure? Try a preview TRAIN NOWOnline Tactical Casualty Care Classes
Notes:
*For those unfamiliar with this term, BLUF is “Bottom Line Up Front,”
1 Deakin CD, Low JL. Accuracy of the advanced trauma life support guidelines for predicting systolic blood pressure using carotid, femoral, and radial pulses: observational study. BMJ. 2000;321(7262):673-674.
2 Wall PL, Buising CM, Grulke L, Troester A, Bianchina N, White S, Freymark R, Hassan A, Hopkins JW, Renner CH, Sahr SM. Effectiveness of Pulse Oximetry Versus Doppler for Tourniquet Monitoring. J Spec Oper Med. 2017 Spring;17(1):36-44.
Dr. Mike Shertz is the Owner and Lead Instructor at Crisis Medicine. Dr. Shertz is a dual-boarded Emergency Medicine and EMS physician, having spent over 30 years gaining the experience and insight to create and provide his comprehensive, science-informed, training to better prepare everyday citizens, law enforcement, EMS, and the military to manage casualties and wounded in high-risk environments. Drawing on his prior experience as an Army Special Forces medic (18D), two decades as an armed, embedded tactical medic on a regional SWAT team, and as a Fire Service and EMS medical director.
Using a combination of current and historical events, Dr. Shertz’s lectures include relevant, illustrative photos, as well as hands-on demonstrations to demystify the how, why, when to use each emergency medical procedure you need to become a Force Multiplier for Good.



