
EMMA Capnography: Enhancing EtCO2 Monitoring in Respiratory Care
- Posted by Mike Shertz MD/18D
- Categories (C) Circulation, (R) Respiration
To truly understand a casualty’s respiratory status, a provider needs to know both their hemoglobin oxygen saturation, which is easily measured with pulse oximetry, and exhaled carbon dioxide level, a marker of ventilation.
Among changes in the 25 JAN 2024 TCCC guidelines is the requirement to use end-tidal CO2 (EtCO2) monitoring to verify successful placement of a surgical airway in a casualty. Also recommended is frequent and periodic re-assessment of EtCO2, pulse oximetry, and airway patency.
Disclaimer: This post is not sponsored or endorsed by Masimo or any other equipment manufacturer. Crisis Medicine does not accept funding from industry and has no disclosures.
The EMMA capnograph is one of few small, portable, simple, lightweight (2.1 oz with batteries) and aid bag friendly options. This device samples end-tidal CO2 directly out of the casualty’s breath in what is called a “mainstream sample,” which is felt to be more accurate than some other sampling techniques.
EtCO2 is measured by a beam of infrared light projected through the exhaled gas. CO2 absorbs infrared light, which the device can then calculate to EtCO2 in the exhalation. However, because the device uses light transmission through the exhaled breath, significant secretions or moisture in the tube can obviously affect that reading.
The EMMA airway adapter tube, through which the device samples breath, is small and can fit in a typical airway circuit. If the casualty is being ventilated, it can attach directly between the surgical airway / endotracheal tube and the resuscitation bag. Similarly, it can be attached between a mask and resuscitation bag for mask ventilation. It is particularly advantageous here as it can give an indication of a faulty mask seal while providing BVM ventilation.
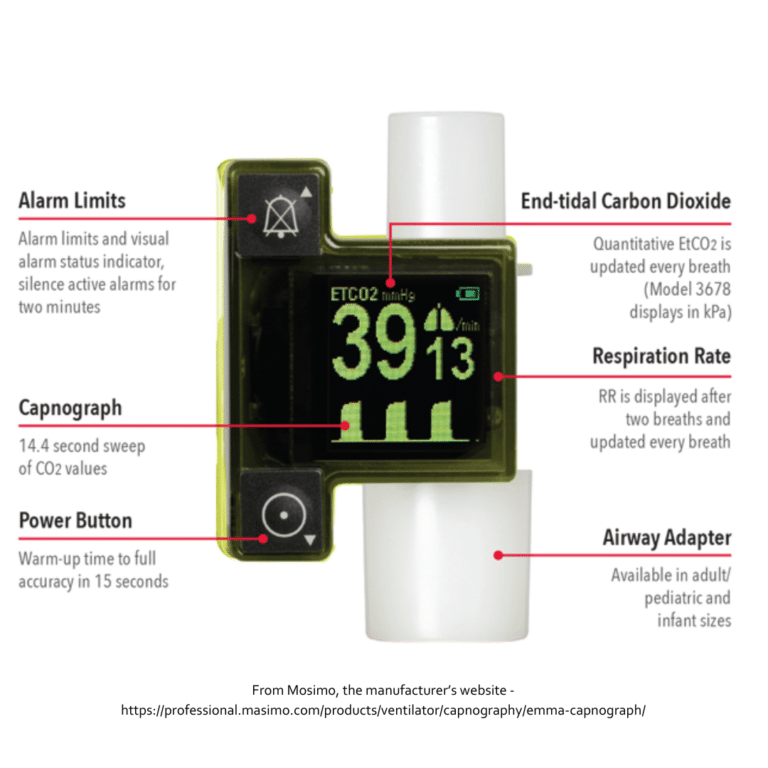
The EMMA device display will show EtCO2 values 15 seconds after being powered on and average those values with each breath. EtCO2 waveform and respiratory rate are also displayed. The only two buttons on the device are to turn it on and to silence or adjust the alarm values.
The factory alarm settings are for a respiratory rate less than 3 breaths per minute (20 seconds of apnea) or an EtCO2 higher than 50 mmHg (7.0kPa). Although these can be changed, anytime the device turns off, it reverts to the factory settings.
Once turned on, the EMMA will switch itself off if no breathing is detected for 2 minutes or after 15 seconds when the device is removed from the airway adapter tube. The device has a continuous run time of ten hours with lithium AAA batteries. (This decreases to 5 hours with alkaline batteries.) In general, alkaline batteries are a terrible idea in expensive devices because of their corrosion risk.
How accurate is the EMMA device? The manufacturer claims it can display an EtCO2 from 0 to 40 mmHg +/- 2 mmHg. Once the EtCO2 exceeds 41 mmHg, the accuracy drops to within 6% of the actual value. Those numbers are consistent with a study of 9 EMMAs tested against a wide range of EtCO2 values in a breathing researcher. Additionally, the authors tested the devices with both fresh and used batteries. The results were the same.1 A Japanese study of 12 anesthetized patients showed similar accuracy.2 Values up to 99 mmHg can be displayed and the device can operate at altitudes of up to 4000 meters.
Even among 50 mechanically ventilated respiratory failure patients in an Egyptian hospital, the EMMA EtCO2 value was within 2 to 7 mmHg of the patient’s actual material EtCO2 measured by arterial blood gas. This range isn’t felt to be clinically significant, and overall, the EMMA correlated well with ABGs.3 A study of 35 general anesthesia patients showed similar results.4
The EMMA capnograph was used for 22 females undergoing breast surgery, all ventilated by BVM for at least twenty minutes. The EMMA EtCO2 values were once again consistent with venous blood gas values.5
EtCO2 monitoring is the gold standard for verifying correct invasive airway placement. Overall, the EMMA capnograph seems to be an accurate and easy way to monitor end-tidal CO2 and a casualty’s ventilation status.
If you’d like an easy read on everything capnography can do for your patient care this review by Masimo, the manufacturer of the EMMA, is very approachable.
References:
1Hildebrandt T, Espelund M, Olsen KS. Evaluation of a transportable capnometer for monitoring end-tidal carbon dioxide. Anaesthesia. 2010 Oct;65(10):1017-21. doi: 10.1111/j.1365-2044.2010.06499.x. PMID: 21198468.
2Kameyama M, Uehara K, Takatori M, Tada K. [Clinical usefulness of EMMA for monitoring end-tidal carbon dioxide]. Masui. 2013 Apr;62(4):477-80. Japanese. PMID: 23697207.
3Zoair H, Ewis A, Ezzat I. Correlation of End-Tidal Carbon Dioxide Tension with Arterial Carbon Dioxide Tension in Patients with Respiratory Failure on Mechanical Ventilation. Egyptian J Hospital Medicine. January 2019. Vol. 74 (8)1902-1906.
4Kim KW, Choi HR, Bang SR, Lee JW. Comparison of end-tidal CO2 measured by transportable capnometer (EMMA™ capnograph) and arterial pCO2 in general anesthesia. J Clin Monit Comput. 2016 Oct;30(5):737-41. doi: 10.1007/s10877-015-9748-x. Epub 2015 Aug 12. PMID: 26264607.
5Lindström V, Svensen CH, Meissl P, Tureson B, Castrén M. End-tidal carbon dioxide monitoring during bag valve ventilation: the use of a new portable device. Scand J Trauma Resusc Emerg Med. 2010 Sep 14;18:49. doi: 10.1186/1757-7241-18-49. PMID: 20840740; PMCID: PMC2949667.
Dr. Mike Shertz is the Owner and Lead Instructor at Crisis Medicine. Dr. Shertz is a dual-boarded Emergency Medicine and EMS physician, having spent over 30 years gaining the experience and insight to create and provide his comprehensive, science-informed, training to better prepare everyday citizens, law enforcement, EMS, and the military to manage casualties and wounded in high-risk environments. Drawing on his prior experience as an Army Special Forces medic (18D), two decades as an armed, embedded tactical medic on a regional SWAT team, and as a Fire Service and EMS medical director.
Using a combination of current and historical events, Dr. Shertz’s lectures include relevant, illustrative photos, as well as hands-on demonstrations to demystify the how, why, when to use each emergency medical procedure you need to become a Force Multiplier for Good.




