What the evidence really shows… Debunking the myth of “dropping a knee;” verb choice matters.
- Posted by Mike Shertz MD/18D
- Categories (M) Massive Hemorrhage, Improvised
🕖 Reading Time, 4 minutes
Manual inguinal compression of the vasculature can work to occlude distal arterial blood flow.
It may not constantly occlude during the entire time the rescuer is applying pressure and might require “readjustment” of the rescuer’s compression to keep occlusion, but it does occlude.
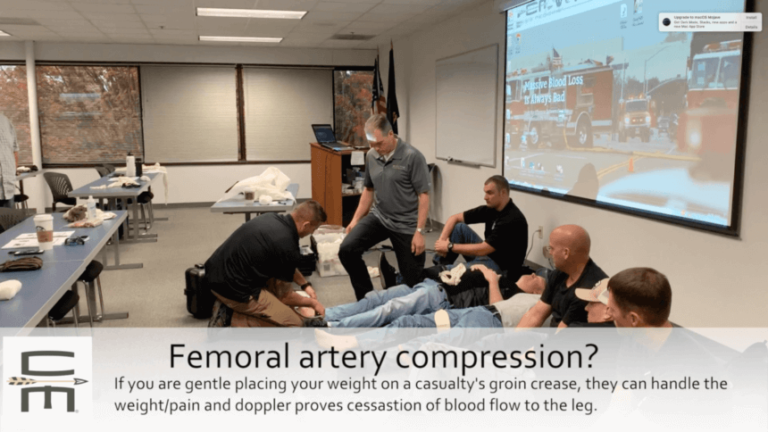
The problem with “dropping a knee” was the force rescuers used to quite literally “drop” their body weight into the inguinal grove.
This caused resultant casualty pain, even in those uninjured and practicing the technique in training. This led to a belief the technique did not work. However, it definitely does work, and if pressure is applied gradually, it is very well tolerated. Consider the verb “placing a knee” as a more successful choice.
Is there a possibility the casualty also has a broken pelvis, and any inguinal pressure could worsen pelvic fracture bleeding? Yes, that could happen. That is why I won’t use the technique every time I deal with bleeding from a lower extremity.
How frequently do pelvic fractures occur in casualties with lower extremity traumatic amputations? 16% in casualties with one above-the-knee thigh amputation and 30 to 32% if the casualty has bilateral lower extremity amputations, based on a US DOD performance improvement project.
However, instead of literally watching the casualty bleed out rapidly from a distal limb injury, I might try and decrease their life-threatening bleeding with inguinal compression. Saving ammunition while trying to survive the current gunfight in order to have more in case there is another one later misses the point. Treat obvious life threats as you find them. Yes, there is “do no harm,” but allowing your casualty unnecessary blood loss seems pretty harmful too.
The decision matrix is pretty straightforward: Which bleeding site do you want to have kill your casualty? The one you can see and are certain is there, or the one that “might be.”
Don’t believe me, look at the data.
One study from 2009 is often cited as to why the technique doesn’t work, but it did, just not well. Manual compression of the common femoral artery in the groin was successful in a study in eight out of ten applications. However, flow returned in 80% at about 21 seconds on Doppler. Swan KG Jr, Wright DS, Barbagiovanni SS, Swan BC, Swan KG. Tourniquets revisited. J Trauma. 2009 Mar;66(3):672-5.
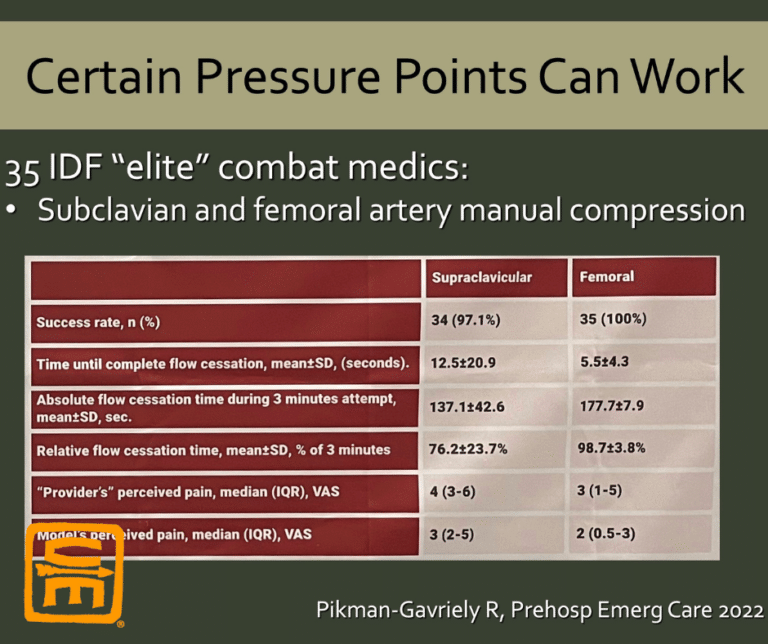
Later studies show markedly more success.
Two Ju Jitsu practitioners were able to reduce mean arterial flow through the femoral artery by 78%, as verified by Doppler ultrasound in 11 volunteers. Although not complete resolution of blood flow past the shin they placed across the inguinal grove, it would substantially reduce distal bleeding.1
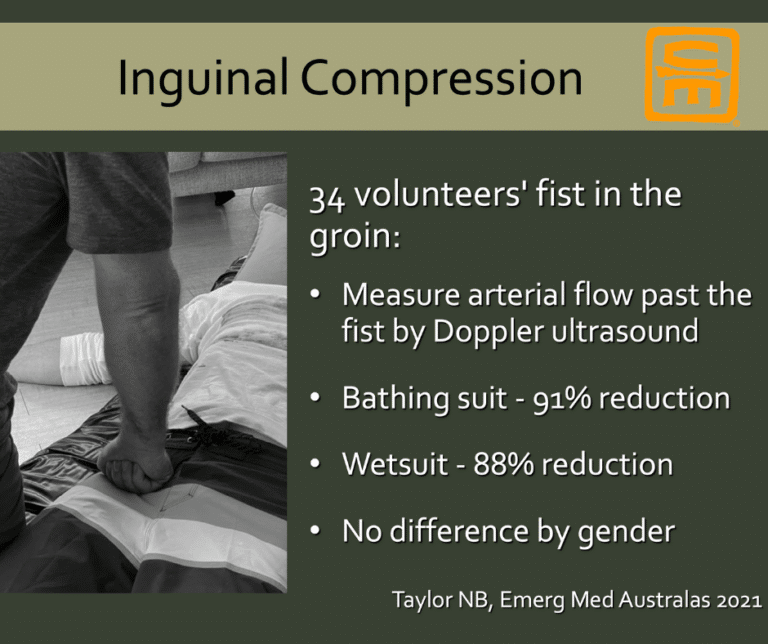
34 volunteers in Australia put a fist in each other’s groin, with and without wetsuits. They showed a 88 to 91% reduction in distal blood flow.2
Finally, 35 IDF “elite” combat medics were able to manually compress each other’s femoral artery with a 100% success rate. However, once again, distal pulses returned periodically, requiring repositioning of the rescuer. Over a three-minute hold in the groin, flow was occluded for 177 seconds, resulting in an overall elimination of flow for three minutes 98.7% of the time.3
Conclusion? If the casualty has a mangled pelvis, I might not use this technique, but I want to save the casualty from the injury I can see is killing them.
For more information on this topic, you can see the article at the website, which discusses the anatomy and our anecdotal data.
References
1Swan KG Jr, Wright DS, Barbagiovanni SS, Swan BC, Swan KG. Tourniquets revisited. J Trauma. 2009 Mar;66(3):672-5.
2Taylor NB, Lamond DW. Stopping Haemorrhage by Application of Rope tourniquet or inguinal Compression (SHARC study). Emerg Med Australas. 2021 Oct;33(5):803-807.
3Pikman Gavriely R, Lior Y, Gelikas S, Levy S, Ahimor A, Glassberg E, Shapira S, Benov A, Avital G. Manual Pressure Points Technique for Massive Hemorrhage Control-A Prospective Human Volunteer Study. Prehosp Emerg Care. 2022 Sep 28:1-6.
Dr. Mike Shertz is the Owner and Lead Instructor at Crisis Medicine. Dr. Shertz is a dual-boarded Emergency Medicine and EMS physician, having spent over 30 years gaining the experience and insight to create and provide his comprehensive, science-informed, training to better prepare everyday citizens, law enforcement, EMS, and the military to manage casualties and wounded in high-risk environments. Drawing on his prior experience as an Army Special Forces medic (18D), two decades as an armed, embedded tactical medic on a regional SWAT team, and as a Fire Service and EMS medical director.
Using a combination of current and historical events, Dr. Shertz’s lectures include relevant, illustrative photos, as well as hands-on demonstrations to demystify the how, why, when to use each emergency medical procedure you need to become a Force Multiplier for Good.