Landmine Umbrella: Not for a day at the beach
- Posted by Mike Shertz MD/18D
- Categories (M) Massive Hemorrhage, MARCH
🕖 Reading Time, 9 minutes
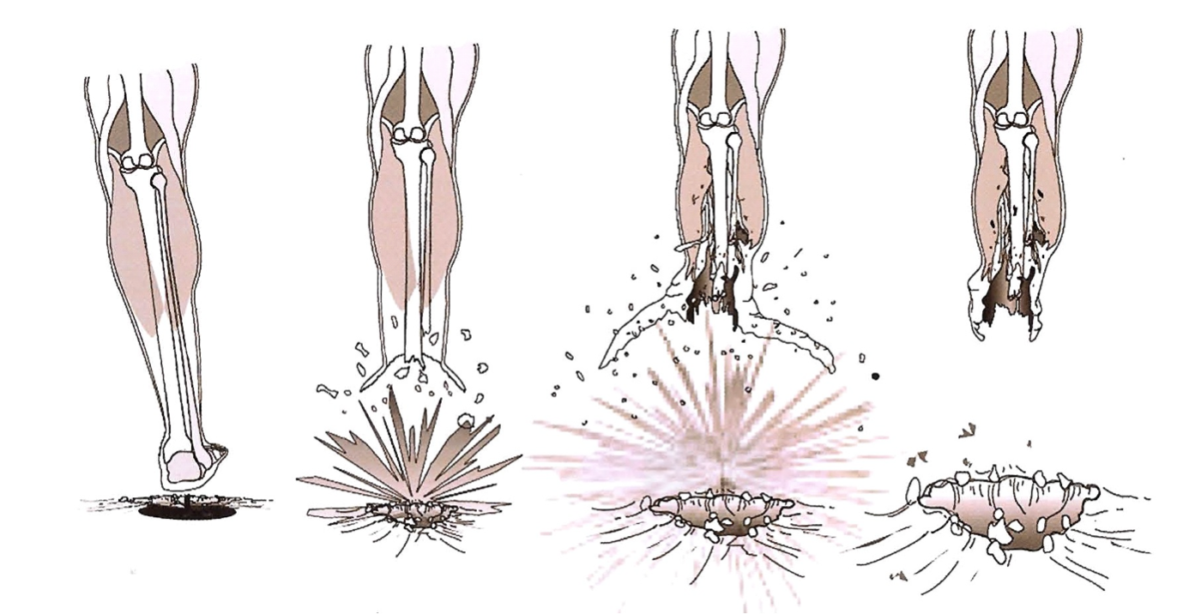
When a casualty steps on a blast mine or is very close to an explosive charge, the explosive force travels up the leg/limb of the casualty stripping skin, fascia, and muscle off the bone. This is similar to “blunt dissecting” in medicine, where we use fingers or a hand to separate tissue along fascial plains. How is this important to casualty management? The partially detached skin, muscle, and fascia expand up and out from the foot/leg like opening an umbrella, hence the term “landmine umbrella.” The resulting injury extends much more proximally (up the limb) than initially clinically apparent.
Once the pressure wave dissipates, the partially detached and expanded tissue “flops” back down around the remaining leg, like closing an umbrella. Sometimes, this tissue can appear viable and leads rescuers to place a tourniquet for the amputation, but improperly just a few inches proximal to the apparent amputation, without realizing the actual tissue destruction goes much higher, generally to the knee joint. The tissue plains in the knee and above are more affixed and harder to “blunt dissect” off, so the umbrella tends to stop at this location. Since this tourniquet placement is below devitalized tissue, the risk for massive hemorrhage occurring from the transected arteries remains.
Massive bleeding from a fully transected artery doesn’t always occur immediately after injury secondary to vasospasm, arterial retraction if fully severed, and wound mechanics. Massive hemorrhage can begin later, when rescuers are transporting the patient or have gone on to another casualty for triage, potentially causing them to miss the patient’s bleeding.
To eliminate this concern, the rescuer needs to identify when a landmine umbrella injury might have occurred. The easiest clue is when the remaining injured leg is much bigger in circumference than the uninjured leg.
Although the simple answer can be to go “high and tight” with the initial tourniquet application, eventually someone will have to convert the tourniquet distally and this becomes an issue. Where does the conversion properly go?
Rarely does a trauma manikin identify this detail in a training aid. Most amputated legs on manikins shown no swelling or tissue expansion which can provide the student with a training scar
Recently, while at the Special Operations Medical Scientific Assembly, I saw a trauma training manikin called a “Simbody” from Prometheus Medical. The leg amputation demonstrated the enlargement that occurs with the landmine umbrella. This is the first training tool I’ve seen that provided this level of detail.
Training aides provide training, both intentional and unintended, which is why trainers need to understand the details.
Note: War Surgery in Afghanistan and Iraq: A series of cases, 2003 -2007. Office of the Surgeon General. Borden Institute. 2008
Dr. Mike Shertz is the Owner and Lead Instructor at Crisis Medicine. Dr. Shertz is a dual-boarded Emergency Medicine and EMS physician, having spent over 30 years gaining the experience and insight to create and provide his comprehensive, science-informed, training to better prepare everyday citizens, law enforcement, EMS, and the military to manage casualties and wounded in high-risk environments. Drawing on his prior experience as an Army Special Forces medic (18D), two decades as an armed, embedded tactical medic on a regional SWAT team, and as a Fire Service and EMS medical director.
Using a combination of current and historical events, Dr. Shertz’s lectures include relevant, illustrative photos, as well as hands-on demonstrations to demystify the how, why, when to use each emergency medical procedure you need to become a Force Multiplier for Good.



