Shock Index: a more sophisticated determinant of hypovolemic shock
- Posted by Mike Shertz MD/18D
- Categories (C) Circulation, MARCH
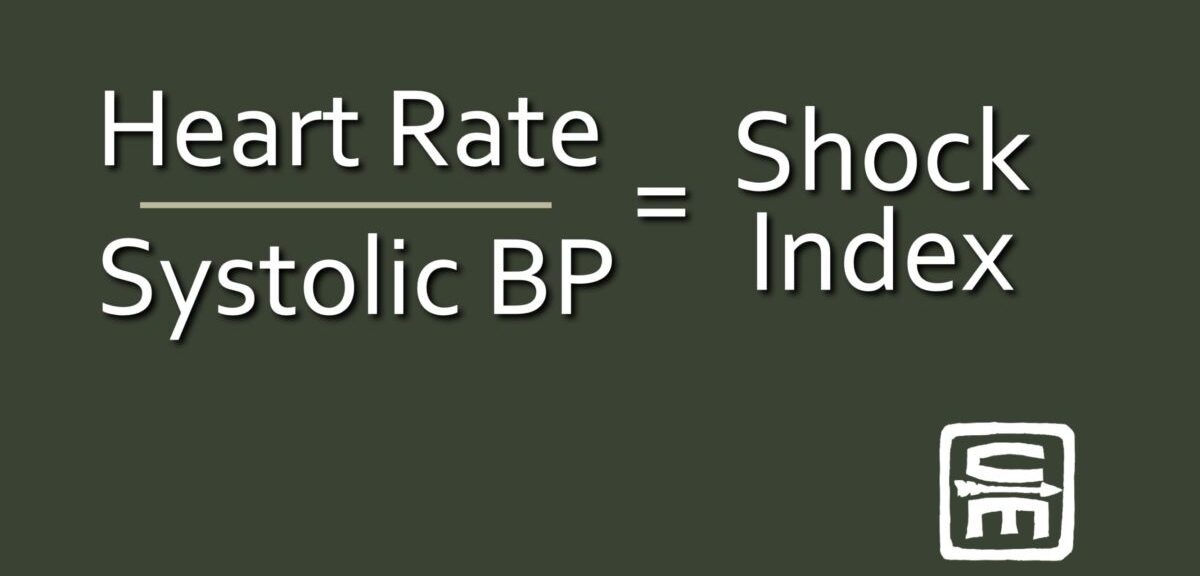
Although not as convenient as evaluating the “Go / No Go” presence of a casualty’s radial pulse, their “shock index” is a much more sophisticated snapshot of their hypovolemic status. Shock index is a ratio of the trauma patient’s heart rate divided by their systolic blood pressure.Simply put, anytime a casualty’s heart rate is higher than their systolic blood pressure, that’s bad.
Initially proposed in 1967, the shock index has recently gained favor as a more reliable predictor of hypovolemia in trauma patients than the heart rate or blood pressure alone.
In concept, as a patient loses blood, their heart rate should increase to circulate the remaining volume faster. In trauma patients with systolic blood pressures less than 90 mmHg, only 71% also have heart rates over 100 beats per minute.1 Unfortunately, that means despite being hypotensive, nearly 1/3 of trauma patients have normal heart rates. This isn’t just a byproduct of the prevalence of antihypertensive medications but is just how some patients respond to hypovolemia.
Interestingly, when healthy volunteers donate 450 ml of blood, their heart rate and systolic blood pressure remains in the normal range after donation; however, their shock index increases.
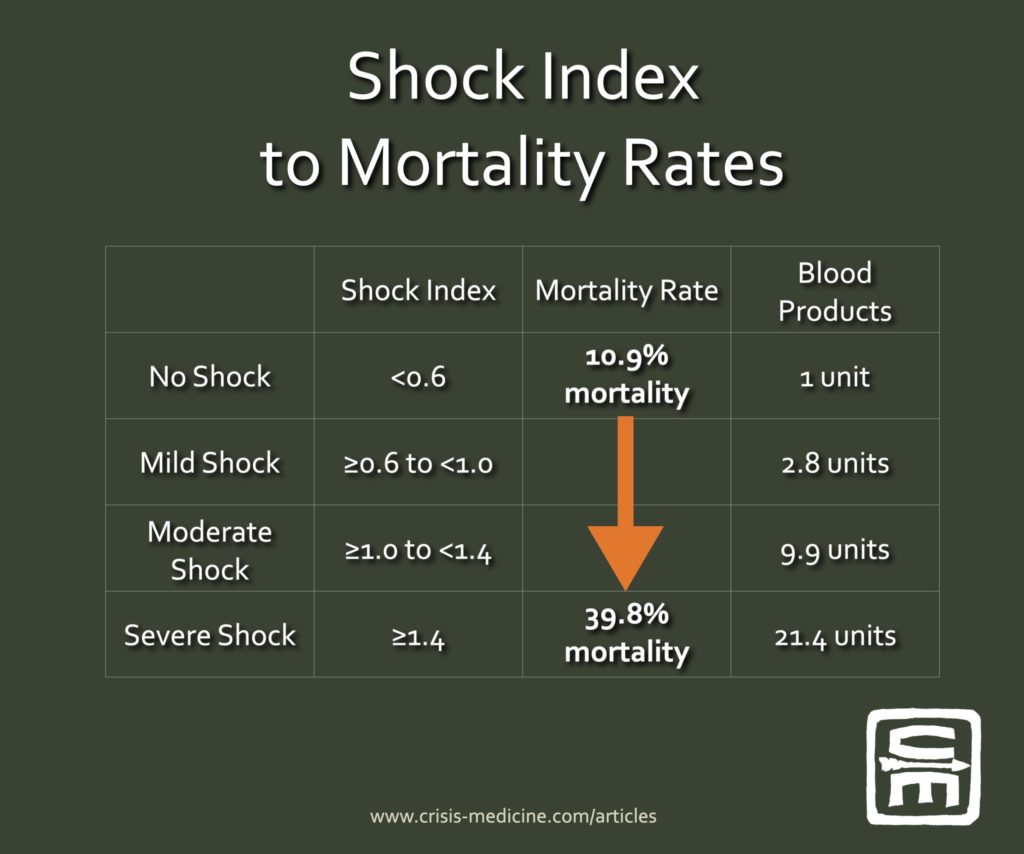
Shock index (SI) is broken into four groups:
no shock is a SI of <0.6,
mild shock ≥0.6 to <1.0,
moderate shock ≥1.0 to <1.4,
and severe shock ≥1.4.
Applying this concept to 21,853 trauma patients in a German registry showed that as a patient’s shock index increases, they have a corresponding increase in mortality, trauma-induced coagulopathy, transfusion requirement, the likelihood of massive transfusion (more than ten units of blood in the first 24 hours), and higher rates of intubation.2 The patients with a normal shock index (<0.6) had a 10.9% mortality and received on average one unit of blood. In the group with severe shock (≥1.4), the mortality rate increased to 39.8% and received an average of 21.4 units of blood.
Casualties with a SI of ≥1.4 are twenty-times more likely to receive a massive transfusion. There is also a fivefold increase in mortality if the casualty’s SI increases ≥0.3 between prehospital and ED readings.
Though most studied in trauma patients, literature showing the shock index is also valid in gastrointestinal bleeds and ruptured ectopic pregnancies.
Because children have higher heart rates and lower systolic blood pressures at baseline, the shock index can’t be used as-is for pediatrics. There are a few studies applying an adjusted version to pediatric trauma, but as significant pediatric trauma is unusual and largely blunt trauma, this literature is evolving.
Operationally: if you have a blood pressure cuff, this is a more sophisticated way to evaluate shock. Most TECC/TCCC situations will not have a BP cuff present; however, if there is one available while awaiting transport, it can be used to guide prehospital care.
Interested to learn more? Try our online courses, or get started with a sample of the material in the preview course
Preview CourseNot sure? Try a preview TRAIN NOWOnline Tactical Casualty Care Classes
References
1 Demetriades D, Chan LS, Bhasin P, Berne TV, Ramicone E, Huicochea F, Velmahos G, Cornwell EE, Belzberg H, Murray J, Asensio JA. Relative bradycardia in patients with traumatic hypotension. J Trauma. 1998 Sep;45(3):534-9.
2 Mutschler M, Nienaber U, Münzberg M, Wölfl C, Schoechl H, Paffrath T, Bouillon B, Maegele M; TraumaRegister DGU. The Shock Index revisited – a fast guide to transfusion requirement? A retrospective analysis on 21,853 patients derived from the TraumaRegister DGU. Crit Care. 2013 Aug 12;17(4):R172.
Dr. Mike Shertz is the Owner and Lead Instructor at Crisis Medicine. Dr. Shertz is a dual-boarded Emergency Medicine and EMS physician, having spent over 30 years gaining the experience and insight to create and provide his comprehensive, science-informed, training to better prepare everyday citizens, law enforcement, EMS, and the military to manage casualties and wounded in high-risk environments. Drawing on his prior experience as an Army Special Forces medic (18D), two decades as an armed, embedded tactical medic on a regional SWAT team, and as a Fire Service and EMS medical director.
Using a combination of current and historical events, Dr. Shertz’s lectures include relevant, illustrative photos, as well as hands-on demonstrations to demystify the how, why, when to use each emergency medical procedure you need to become a Force Multiplier for Good.