START, SALT, and RAMP Triage in a Mass Casualty Event
- Posted by Mike Shertz MD/18D
- Categories (C) Circulation, MARCH, More
Triage systems are used by prehospital providers to “sort” casualties
🕖 Reading Time, 12 minutes
into essentially those who are dead or will likely die despite treatment, those with injuries that don’t really require prehospital treatment, and those with injuries that are immediately life-threatening and likely to die without rapid intervention. Three of the most common systems are START, SALT, and what is known as RAMP. Do these “different systems” actually result in markedly different final triage categories when applied to MCI casualties?
Operations Order – “Operation Hyperglycemia”
Situation: A prolific gingerbread bomb maker has been terrorizing Christmas town. He has detonated several devices recently and sources indicate he plans for more. He has a pregnant wife and young child. All reside in a small gingerbread house.
Mission: Arrest the gingerbread bombmaker.
Execution: Your law enforcement gingerbread tactical team will execute an early morning no knock arrest warrant at his home.
Service and Support: One tactical medic has been attached to the LEO tactical team for this operation.
Command and Signal: Per unit SOP.
On the twelve days of Christmas, Crisis Medicine brought to me, triaging a mass casualty…
Mass casualty scenes are chaotic. Overwhelmingly, complicated triage systems are difficult to put into practice by the cognitively overloaded responder. Because of this, rarely, if ever, are actual triage systems truly used during an event. This has led to an ongoing quest for the optimal and usable triage system.
Follow along over the next series of posts to see all three triage systems applied to a gingerbread MCI.

Once the gingerbread bomb maker detonated his device, law enforcement, neighbors, and his own family were wounded. To evaluate the casualties and compare the triage systems, we’ll need to have the diagrams of all three close at hand (click the diagram to follow the links and get a full-sized version):
START (Simple Triage And Rapid Treatment)
divides casualties into four categories: expectant (already dead or going to die regardless), immediate (need help now), delayed (can wait a while for treatment), and minor (take yourself to the hospital, you’ll be fine). START has been criticized as difficult to implement as it requires taking a respiratory rate or evaluating capillary refill. These categories are often color-coded into black (expectant), red (immediate), yellow (delayed), and green (minor), respectively.
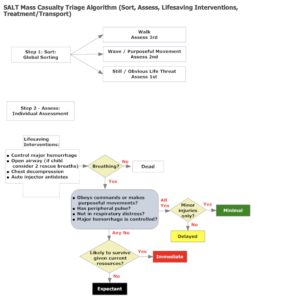
SALT (Sort, Assess, Lifesaving interventions, and Treatment / Transport)
divides casualties into five categories: dead (already), expectant (essentially going to die regardless), immediate (need help now), delayed (can wait a while for treatment), and minimal (take yourself to the hospital, you’ll be fine). These categories are often color-coded into “dead”, black (expectant), red (immediate), yellow (delayed), and green (minimal), respectively. The CDC supports it as the most scientifically designed triage method.
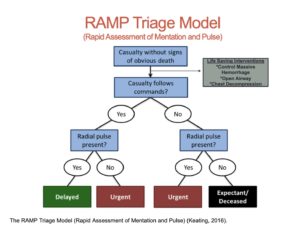
RAMP (Rapid Assessment of Mentation and Pulse)
divides casualties into three categories: expectant / deceased (already dead or going to die regardless), urgent (need help now), or delayed (you don’t need help right this second). These categories are often color-coded into black (expectant or deceased), red (urgent), and green (delayed), respectively. It essentially is similar to the Field Triage Score. For those not familiar with RAMP triage, Brad Keating presented to the TECC committee November 2019.
Print the full-sized diagrams to follow along and triage the unfortunate gingerbread casualties over the coming week.
In the first group of casualties, three SWAT officers are wounded, one with an isolated head injury, one with an abdominal injury, and one with massive hemorrhage secondary to an amputated leg.

- The head-injured officer: is not moving, doesn’t follow commands, has a respiratory rate of 20, and has a palpable radial pulse.
- The officer with a penetrating abdominal injury: is walking, follows commands, has a respiratory rate of 26, and a palpable radial pulse.
- The officer with a leg amputated: is crawling, follows commands, has a respiratory rate of 28, and a palpable radial pulse.
How do you triage these casualties under each of the triage systems?
In applying the three triage systems to our gingerbread mass casualty, the first three wounded triage as follows:
- The head-injured officer:
SALT → still – first evaluated, breathing, doesn’t follow commands, = Immediate or expectant based on resources
RAMP →Doesn’t follow commands, has a palpable radial pulse = URGENT
- The officer with a penetrating abdominal injury:
SALT → walking = assessed third; follows commands, palpable radial pulse. Minor injury? NO = DELAYED
RAMP → Follows commands & has radial pulse = DELAYED
- The officer with a leg amputated:
SALT → crawling with obvious life threat = assessed first, lifesaving intervention = place tourniquet, is breathing, has more than minor injuries but hemorrhage is controlled = DELAYED
RAMP → follows commands & has a palpable radial pulse = DELAYED

As the bombmaker was completely blown apart, he would not get triaged. His injuries are “incompatible with life.” However, if he were still alive, he should be triaged the same as any other casualty. That is, once he has been secured and searched for the safety of rescuers. Rescuers can’t “under triage” him simply because he is the primary bad actor in this event. Not all may agree, but LEO agencies have been sued over this precise issue historically.

In the second group of casualties, a SWAT officer suffered blast lung from over pressure, a passerby was wounded by shrapnel, and a law enforcement K9 suffered an amputated rear limb.
- Officer: crawling and following commands, respiratory rate of 40, a palpable radial pulse.
- Passerby: walking, following commands, respiratory rate 14, with a palpable radial pulse
- K9: crawling, shrieking, following commands, respiratory rate 26, with a palpable femoral pulse.
In applying the three triage systems to our next three wounded gingerbread casualties, they sort as follows:
- Officer with blast lung
SALT → moving = assessed second; likely undergo chest decompression (which will not fix his injuries), breathing and in respiratory distress = IMMEDIATE or EXPECTANT based on resources RAMP → follows commands, palpable radial pulse = DELAYED
- Passerby:
SALT → walking = assessed third; breathing, minor injuries only = MINIMAL
RAMP→ follows commands, has a radial pulse = DELAYED
- K9
START → ? SALT → ? RAMP → ?

How do you integrate a law enforcement K9 among multiple human victims? The DOD K9 TCCC guidelines state: “Triage casualties as required. Human casualties should always be given priority over MWD (military working dog) casualties.” Does a severely wounded K9 triage higher than the delayed or minimal human casualties?

In the third group of wounded gingerbread, a SWAT officer has massive hemorrhage from an amputated arm; a neighbor who came out to see what the ruckus was about suffered burns over his arm, leg, and torso; and another SWAT officer is unresponsive with no signs of life.
- Officer with amputated arm: still, not following commands, respiratory rate 36, no radial pulse.
- Passerby with burns: 20% partial thickness body surface area burns; walking, following commands, respiratory rate 14, with a palpable pulse.
- Unresponsive SWAT Officer: still, not following commands, no spontaneous breathing, no pulse.
The three triage systems apply as follows to the next group of gingerbread casualties:
- Officer with amputated arm:
SALT → still and obvious life threat = assessed first; apply tourniquet, breathing but not following commands and nopalpable radial pulse= IMMEDIATE or EXPECTANT depending on resources RAMP → not following commands, no radial pulse = EXPECTANT / DECEASED
- Passerby with burns:
SALT → walking = assessed third, breathing, minor injuries only? Is 20% BSI minor? = MINIMAL or DELAYED depending on that assessment
RAMP → follows commands, has a radial pulse = DELAYED
- Unresponsive officer:
SALT → still = evaluated first; LSI = open his airway, not breathing = DEAD
RAMP → does not follow commands, no pulse = EXPECTANT / DECEASED

None of the systems includes burns. The American Burn Association has triage criteria for burns over 20% Body Surface Area or with inhalational injuries, as injuries that are “significant” and should go to a burn center. In a recent burn MCI article, START was used, but the results were felt to have been “misleading.” Unless the casualty presented with tachypnea, they were often under triaged. Many went on to develop respiratory distress from evolving inhalational injury that was unaccounted for during the first several hours of the event.

In the home, the disgruntled gingerbread bomber blew himself up, wounded his pregnant wife, who suffered a penetrating chest injury, and killed his young son. The next-door neighbor was decapitated in the blast and landed in the back yard. The bomb maker’s body is found scattered across the crime scene. His injuries are incompatible with life; therefore he does not get triaged.
- Pregnant wife: penetrating chest injury, walking, following commands, respiratory rate of 26, palpable radial pulse.
- Bomber’s son: still, not following commands, no spontaneous breathing, no palpable radial pulse.
- Neighbor: still, not following commands, no spontaneous breathing, no palpable radial pulse.
In the last of our triaging the gingerbread MCI, the various triage systems break down as follows:
- Pregnant wife:
START → walking = MINOR
SALT → walking = assessed third (is her chest injury an obvious life threat? If so assessed first); breathing, follows commands, has a palpable radial pulse, but has more than a minor injury = DELAYED
RAMP → follows commands, palpable radial pulse = DELAYED
- Bomber’s son:
START → does not walk, not breathing, airway is opened = EXPECTANT
SALT → still = assessed first; airway is open, apply two rescue breaths, still apneic = DEAD
RAMP → not following commands, no radial pulse = EXPECTANT / DECEASED
- Neighbor:
START → has injuries incompatible with life = do not triage
SALT → has injuries incompatible with life = do not triage
RAMP → has injuries incompatible with life = do not triage

None of the triage systems include pregnancy as a triage modifier. Should they? The pregnant woman comprises two casualties, not just one. There isn’t any operational way to include it as a category until the pregnancy is clearly visible or verbal notification from the woman as to its presence. Also, until the pregnancy is at least twenty weeks, it isn’t viable outside the body. Based on all of this, the simple answer is no. If not anticipated as a possibility ahead of time, we could see an obviously pregnant casualty as a friction point for the rescuer’s decision-making process.
Although there are many different triage systems in use, comparing just three yields some interesting observations across these gingerbread casualties.
Most interesting is that in the end, the three triage systems put the wounded into the same basic categories.
Though the name used by each system might be slightly different, for example, minor vs. minimal, the expectation is the same. That casualty is less sick than the others and can wait reasonably safely to be managed.
An important point to remember is that triage for treatment is not the same as triage for evacuation. The SWAT officer with an amputated leg, is a high priority for treatment and tourniquet placement, but once his hemorrhage is controlled, he can be a delayed evacuation. SALT provides a treatment step, where the other systems generally do not. Newer versions of RAMP have included a treatment step.
Additionally, SALT calls out specific pediatric steps (consider two rescue breaths after opening a child’s airway), whereas the rest don’t address pediatrics specifically. Pediatric specific triage systems do exist, i.e., “Jump START,” but creating a unique system for kids is even more likely to fail in cognitively overloaded rescuers dealing with both adult and pediatric casualties now forced to work between two different systems simultaneously.
SALT also has an interesting nuance where the casualty can be either immediate or expectant depending on “available resources.” This category came up frequently on this set of wound profiles. Although resources are a critical consideration, it doesn’t provide much guidance to the rescuers on the ground trying to figure out what to do with the casualties in front of them.
One nuisance of START is that all walking casualties are designated “minor” and sent to “secondary triage”. However, an isolated GSW to the chest with normal vitals ultimately, by this system, will be at least delayed as that definition includes serious and potentially life-threatening injuries.
In comparing these three triage systems, it quickly becomes obvious the systems frequently end up with the same conclusion or triage categories assigned to each victim. What is equally obvious is that RAMP is the easiest to use as it divides casualties into only three groups by easily determined parameters. Although it is much less studied, it uses similar decision points as the Field Triage Score https://www.crisis-medicine.com/why-do-traditional-triage-systems-fail-in-actual-events/, which we have been teaching as a simpler and effective system to triage casualties in high-risk environments since its publication in 2010.
For more information on triage and review of some recent, provocative triage literature, check out the newer article, Rethinking Triage: Could Intuition Outperform Formal Systems? Also using Gingerbread, of course.
Interested to learn more? Try our online courses, or get started with a sample of the material in the preview course
Dr. Mike Shertz is the Owner and Lead Instructor at Crisis Medicine. Dr. Shertz is a dual-boarded Emergency Medicine and EMS physician, having spent over 30 years gaining the experience and insight to create and provide his comprehensive, science-informed, training to better prepare everyday citizens, law enforcement, EMS, and the military to manage casualties and wounded in high-risk environments. Drawing on his prior experience as an Army Special Forces medic (18D), two decades as an armed, embedded tactical medic on a regional SWAT team, and as a Fire Service and EMS medical director.
Using a combination of current and historical events, Dr. Shertz’s lectures include relevant, illustrative photos, as well as hands-on demonstrations to demystify the how, why, when to use each emergency medical procedure you need to become a Force Multiplier for Good.