Using facial features for proper sizing of an NPA?
🕖 Reading Time, 7 minutes
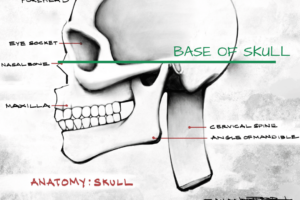
The ability of a nasal pharyngeal airway (NPA) to maintain a patent airway is dependent on both the NPA’s internal diameter and length. Proper placement of a nasal pharyngeal airway ideally involves the tip of the tube about 1 cm from the epiglottis.1
Proper placement allows an air passage through the nose and behind the tongue, which can be a frequent occluder of the airways in patients with altered mental status. If the tube extends past the epiglottis, there is a risk of airway obstruction from the tube itself. If the tube is too short, it might not end behind the tongue and, therefore, not provide the airway patency desired.
As NPA tube diameter and length are related, bigger diameter tubes have longer lengths; therefore, picking the correct size for the patient is important to ensure its tip is properly placed. Within EMS, emergency medicine, and anesthesiology there are multiple different techniques to size NPAs based on your patient’s external facial anatomy.
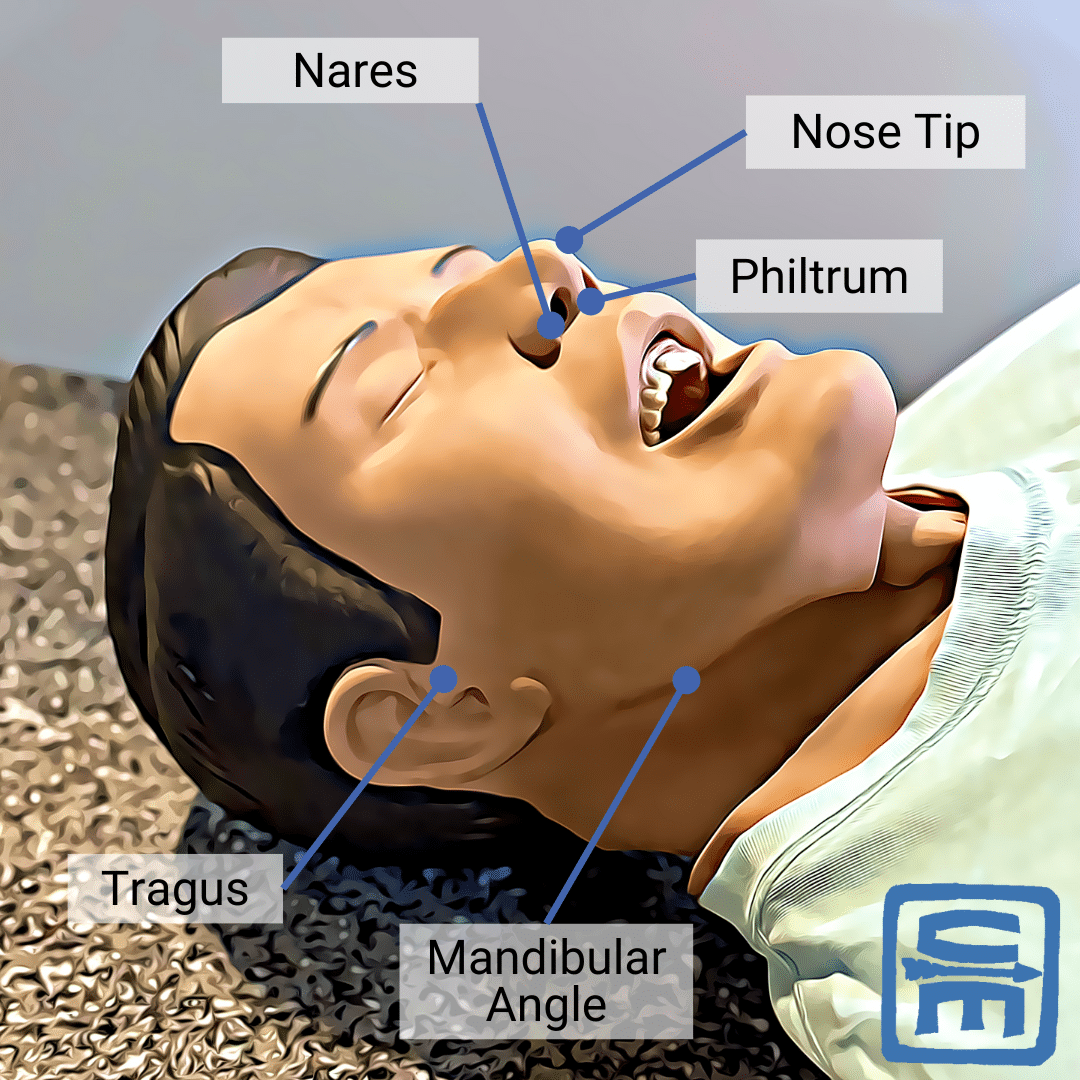
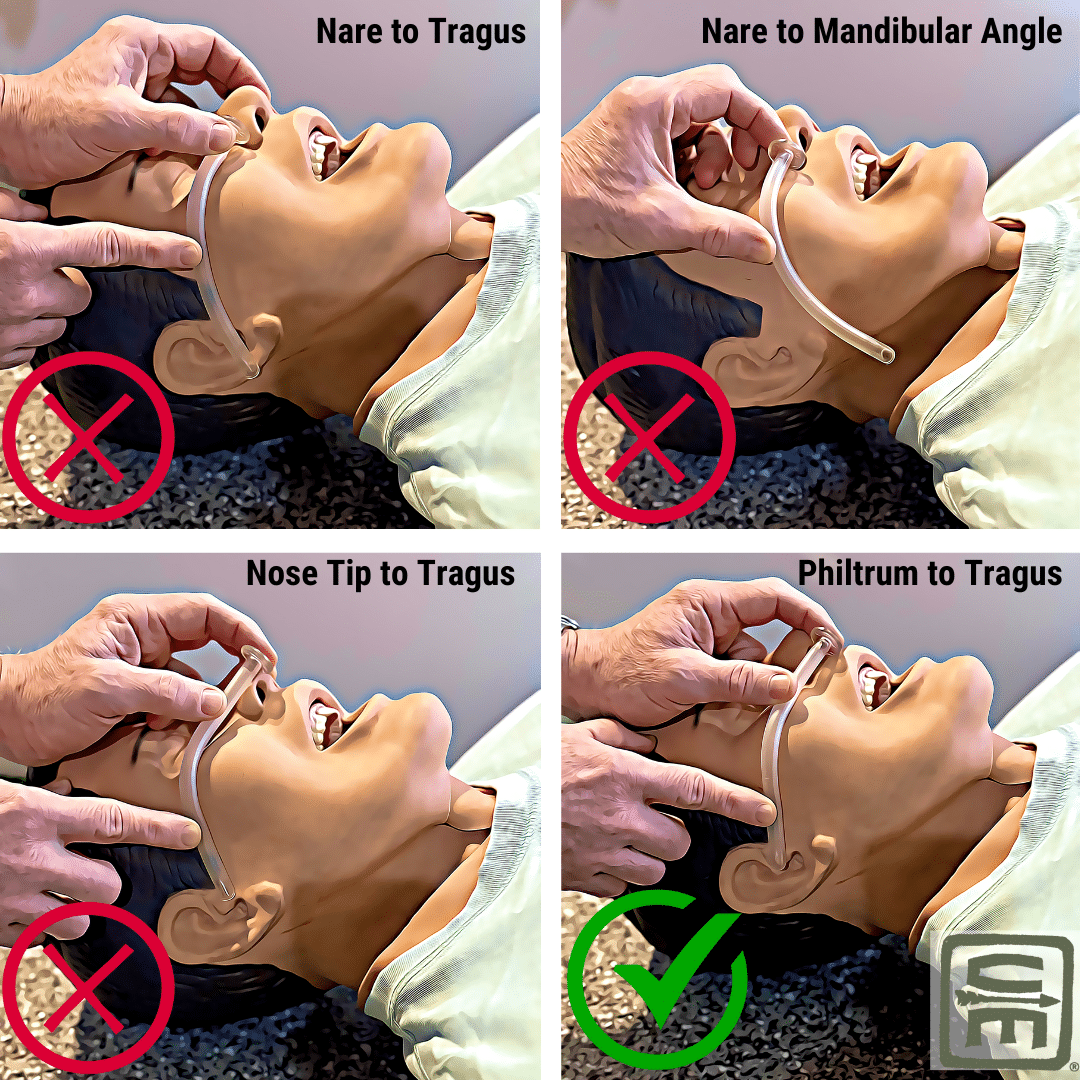
Nose Tip to Ear Tragus or to the Mandibular Angle is Not Predictive
In 1993, 120 men and women undergoing routine surgery had the distance from their nares to epiglottis measured visually via a fiberoptic scope placed through an NPA (7 mm internal diameter (ID) for women and 8 mm ID for men). In 60% of these placements, the tip of the NPA was at or beyond the epiglottis. None met criteria as properly placed. In 13% of the cases, the tip was wedged in the vallecula anterior to the epiglottis, near the vocal cords, and at risk for airway obstruction.1
After making this observation, the author measured patients’ external facial landmarks to determine the best way to choose which size NPA would result in correct placement. Unfortunately, they found no reliable correlation between the distance from the nose tip to the ear tragus or to the mandibular angle (corner of the jaw).1
Diameter of the Patients’ Nares or Little Finger is not Reliable
In 2001, other authors studied ten individuals undergoing MRI to determine if the diameter of the patients’ nares or little finger could be used for sizing. Neither was deemed reliable.2
Nares to Mandibular Angle Distance Does not Accurately Predict
In 2004, 95 general anesthesia patients (50 male, 45 female) had their nares to vocal cord distance measured by fiberoptic scope. The patients’ nares to mandibular angle distance was similar between genders, even with height differences, and did not accurately predict nares to epiglottis distance. The authors suggested the lateral border of the nares to tragus distance was a reliable measure of desired NPA length, with very few predicated NPA lengths being too long. They concluded their results differed from the 1993 study because they used the lateral border of the nare, not the nose tip.7
Neither Nares to Tragus or to Mandibular Angle is Accurate
In 2015, another 100 patients (50% male: female) undergoing elective surgery had their nares to vocal cord distance measured via fiberoptic nasal scope. Neither nares to tragus nor nares to mandibular angle was judged to be accurate. The patients’ arm span or sternal length was most predictive in their study. However, this isn’t operationally useful, as it requires a mathematical formula to convert measured length into a nares to epiglottis distance.3
Philtrum to Tragus is the Most Predictive
Also, in 2015, the largest study to date was published looking at 200 elective surgery patients (86 male, 114 female) whose external facial anatomy was measured with a tape measure. These measurements were then compared to the distance from their nares to epiglottis via fiberoptic nasal scope. They found the difference between correct NPA length and nares to tragus could be off by 1.5 to 3.6 cm, nares to mandibular angle 2.3 to 4.5 cm, and philtrum to mandibular angle 0.6 to 2.6 cm. Their best correlation was philtrum to tragus at only 0.3 to 1.6 cm off. This measurement was off by no more than 2 cm in 97.5% of the study population, and 60% were off less than 1 cm using philtrum to tragus. Subsequently, using this length to size an NPA would result in choosing one that was within 1 cm of ideal in 60% of the patients it is used on.
Although many will say none of these external measurement techniques are accurate enough for actual use6 and NPA size should be determined strictly by patient height, that is difficult operationally, especially when confronted with a horizontal and altered patient.
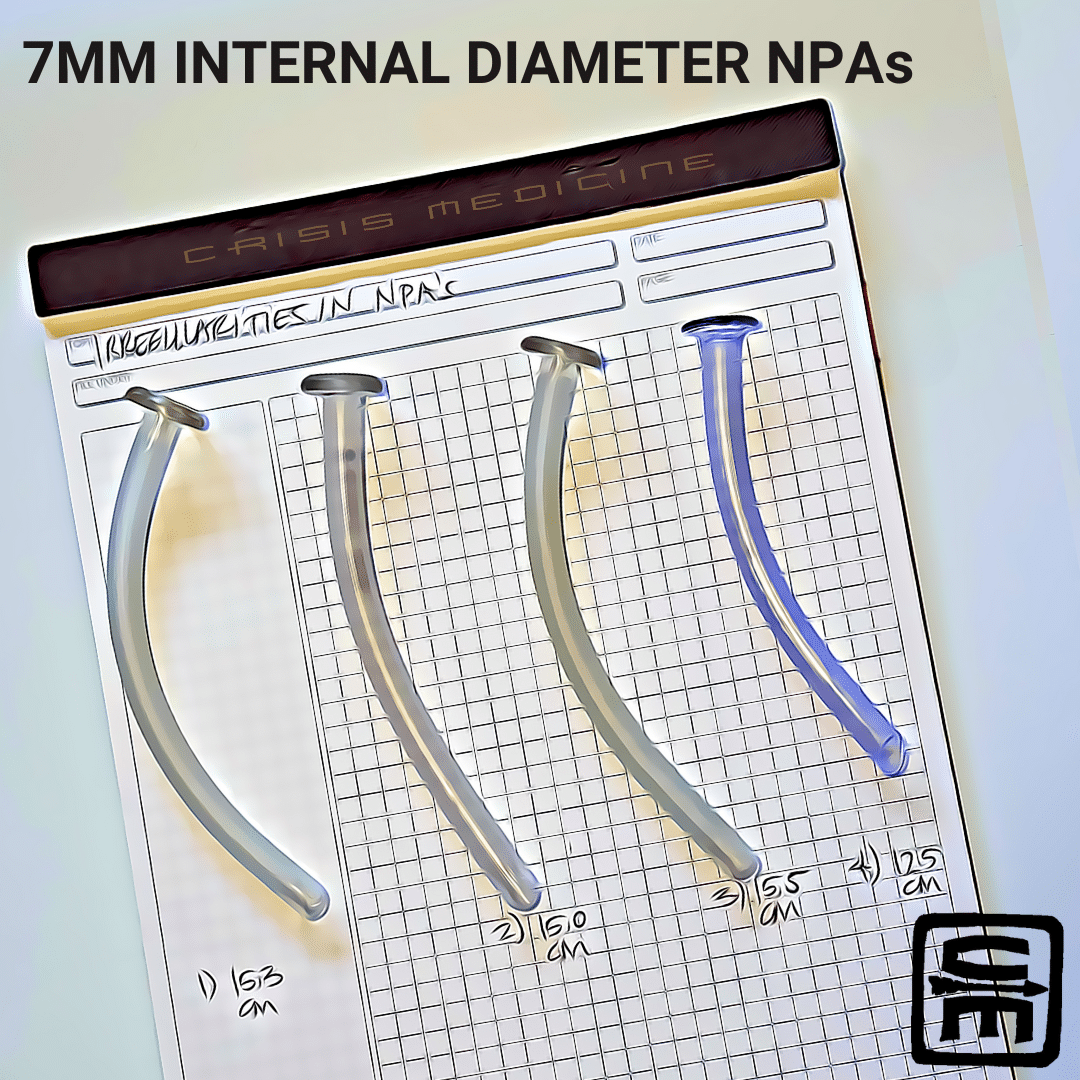
Manufacturing Inconsistencies Complicates Any Preplanning
Further complicating any preplanning is the non-standardized NPA length among various manufacturers and often among the same manufacturer’s different styles of NPAs. This becomes even more difficult to plan for as most manufacturers don’t’ specify the length of their NPAs.5
This problem in lack of standardization is demonstrated clearly by two authors who noted airway obstruction after placement of a 7.0 mm ID NPA into an adult male with traumatic head injury, but then airway patency with a different manufacturer’s 7.0 mm NPA. They found a 37 mm difference in NPA length among five styles and three manufacturers labeled 7.0 mm ID NPAs.5 With optimal NPA placement felt to be the tip 1 cm from the epiglottis, this length variance could easily be clinically significant and either cause airway obstruction from being too long or inadequate patency because it was too short.
Operationalizing NPA Sizing
What does all of this mean? If faced with a patient requiring placement of a nasal pharyngeal airway, the best external sizing technique, based on a study of 200 individuals, would be to use an NPA that extends from the philtrum to the tragus. Since NPA length is more important than diameter for airway patency, this technique eliminates issues with the non-standard manufacturing and labeling length of NPAs.
Impact of Head Tilt or Recovery Position on NPA Size
As a side note, Stoneham also studied 23 men and women undergoing elective surgery with NPAs placed who had their head and neck fully flexed and extended to determine the distance travel of the NPA tip relative to the epiglottis. Despite maximal flexing and extending, the NPA tip only moved 5.7 mm away when flexed and 1.3 mm closer when extended. This degree of movement wasn’t felt to be clinically significant.1
References:
1Stoneham MD. The nasopharyngeal airway. Assessment of position by fibreoptic laryngoscopy. Anaesthesia. 1993 Jul;48(7):575-80. doi: 10.1111/j.1365-2044.1993.tb07119.x. PMID: 8346770.
2Roberts K, Porter K. How do you size a nasopharyngeal airway. Resuscitation. 2003 Jan;56(1):19-23. doi: 10.1016/s0300-9572(02)00291-5. PMID: 12505734.
3Sareen B, Kapur A, Gupta SK, Sareen PB, Nischal H. Clinical evaluation of nares-vocal cord distance and its correlation with various external body parameters. Indian J Anaesth. 2015 Apr;59(4):212-5. doi: 10.4103/0019-5049.154997. PMID: 25937646; PMCID: PMC4408648.
4Tseng WC, Lin WL, Cherng CH. Estimation of nares-to-epiglottis distance for selecting an appropriate nasopharyngeal airway. Medicine (Baltimore). 2019 Mar;98(10):e14832. doi: 10.1097/MD.0000000000014832. PMID: 30855511; PMCID: PMC6417616.
5Dogra N, Dhanda S. The long and short of it: Nonstandardised length of nasopharyngeal airways. Eur J Anaesthesiol. 2021 Nov 1;38(11):1202-1204. doi: 10.1097/EJA.0000000000001567. PMID: 34617923.
6Scheuermann-Poley C, Lieber A. Studies on the Correct Length of Nasopharyngeal Airways in Adults: A Literature Review. J Spec Oper Med. 2021 Fall;21(3):45-50. doi: 10.55460/GGFN-XJEG. PMID: 34529804.
7Han DW, Shim YH, Shin CS, Lee YW, Lee JS, Ahn SW. Estimation of the length of the nares-vocal cord. Anesth Analg. 2005 May;100(5):1533-1535. doi: 10.1213/01.ANE.0000149900.68354.33. PMID: 15845720.